What’s dry socket? | Symptoms | Causes | Diagnosis | Treatment | Home Remedies | Prevention | Risks
Tooth extraction is, definitely, not an enjoyable experience, but sometimes it might be unavoidable to keep the dental system healthy. You might have prepared yourself mentally to endure procedural pain, but what if pain worsens and intensifies after a few days. It may be the symptom of a dry socket, also called alveolar osteitis. Although it is a common complication of tooth extraction, it is still rare with an incidence rate of less than 2%. The occurrence of the condition depends on the type of tooth extraction, and it is more likely to develop after the extraction of wisdom teeth.
What is a Dry Socket?
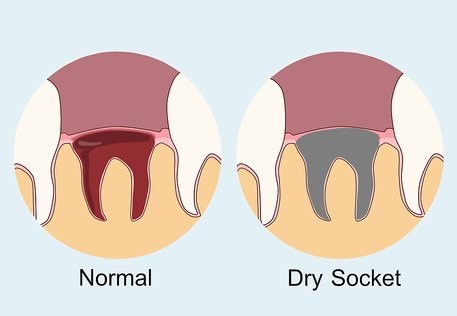
A dry socket is a dental condition linked to tooth extraction, in which intense pain starts 3-4 days after the removal of a tooth. Tooth extraction creates a hole, called a socket, in the jawbone (alveolar bone), in which blood clots to protect nerves and bone underneath. In some cases, this blood clot dissolves or gets dislodged in a few days after tooth extraction. The absence of protective blood clots exposes bone and nerve to fluid, flood, air, and other substances. Direct exposure of bone and nerves to foreign objects causes inflammation, triggering intense pain along with bad breath and a foul taste in the mouth.
Although very rare, the chance of occurrence of dry sockets is relatively high with lower wisdom tooth extraction. Likelihood of occurrence increases manifold if:
- You have a history of dry socket occurrence, as in some cases blood doesn’t clot at the extraction site due to trauma.
- You chew tobacco or smoke cigarettes as nicotine slows healing and the act of inhaling could dislodge the blood clots.
- You are on blood-thinning medication or using oral contraceptives. A high level of estrogen present in contraceptives disrupts the healing process.
- You are not maintaining oral hygiene as per instructions.
What are the symptoms of Dry Socket?
It is very natural to watch the socket side several times in a day, if you notice a dry-looking opening, it could be a symptom of a dry socket. Dislodgement of the blood clots will expose the whitish bone. Here are some symptoms of dry socket onset:
- Acute pain at the site of the tooth extraction
- No blood clot in the socket
- Jawbone will be visible
- Unpleasant breath
- A foul taste in the mouth
- Spread of pain from the tooth hole to eyes, ears, temple, or neck in 2-3 days.
Once the effect of anesthesia drops, you will start to feel moderate pain. But if the pain starts intensifying in the next 2-3 days, you should consult your dentist immediately as it could worsen further, if left untreated in time.
What Causes Dry Socket Development
Blood clot formation is the first step in healing the extracted tooth site. The main cause of dry socket development is loss or non-formation of the blood clot in the socket. This exposes the underlying jawbone and nerves, resulting in inflammation and caused bacterial, mechanical, chemical, and physiological factors.
Bacterial Cause: If the bacteria count in the mouth is high before the tooth extraction due to periodontal disease, it could prevent blood clots. Some bacteria are known for breaking down blood clots.
Chemical Cause: If you chew tobacco or smoke cigarettes, the chance of a dry socket is relative as nicotine decreases the flow of blood in the mouth. If you are smoking after tooth extraction, then it is likely that blood clots won’t form or dislodge.
Mechanical Cause: Excess pressure creation in the mouth by aggressive gargling, sucking through a straw, coughing, or spitting could dislodge the blood clot from the socket.
Physiologic Cause: Genetic factors like hormonal imbalance, jaws anatomy, or medication like contraceptives could prevent blood clot formation.
Whatever is the cause, you should consult your dentist immediately to start treatment in time so that pain could be controlled and the healing process could be reinvigorated.
How is Dry Socket Diagnosed?
If you notice symptoms of dry sockets, you should consult your dentist so that he could start a diagnosis based on your dental treatment history, clinical examination, and symptoms. Timing of the occurrence of symptoms could be a sign of dry socket, as the pain starts increasing after 2-3 days after tooth extraction.
How to Treat Dry Socket?
Dry socket treatment centered on pain management, so your dentist will start with cleaning the socket area to remove any foreign substance. Removal of debris accumulation alleviates the pain and prevents infection spread.
After flushing the socket, your dentist will pack the socket with gauze and medicated gel to numb the pain. To keep pain in check, follow gauze removal instructions as per the advice. Once the gauze is removed, you have to keep the areas clean using a prescribed oral rinse or saltwater.
If required, your doctor might redo the dressing or instruct you to add the new dressing at home. If pain is acute and spread to the ear and eye you can use a cold compress for relief along with non-steroidal anti-inflammatory medications, prescribed by the dentist.
Usually, it takes 6-8 days to treat dry sockets, but if the pain persists you should visit your dentist again after a week. Based on progress, he will suggest measures to prevent infection buildups.
Home Remedies for Dry Socket
Treatment doesn’t end in the clinic as you have to maintain standard oral hygiene to keep the infection in check. Here are some of the most recommended home remedies for dry sockets.
- Your dentist will prescribe gentle flushing of the socket using the medicated solution or saltwater. So, do it as per instruction to get rid of pain caused by the dry socket until the socket heals properly.
- Avoid smoking cigarettes or chewing tobacco to enable speedy healing
- Use lukewarm water to rinse mouth gently, at least 3-4 time a day
- Be careful while brushing as excessive pressure around the affected area could trigger pain
- Drinking plenty of neutral liquids for healing
- Avoid foods that could irritate the socket area
- Use hot and cold packs as per your comfort to relieve pain
How to Prevent Dry Sockets
You are now aware of the dry socket causing factors, so before tooth extractions, you can do the following things to reduce the risk of dry socket conditions:
- Stop chewing tobacco and smoking cigarettes at least a few days before the tooth extraction surgery.
- Consult an experienced dentist who could extract the tooth without causing much discomfort.
- If you are on contraceptive medication, you should inform your dentist in advance so that he could prescribe suitable medication to deal with estrogen.
- Make sure the affected area is properly sterilized and packed.
- Use antibacterial mouthwash or oral gel as prescribed by the dentist
- Consume antibiotic medication without fail
- It takes time to heal, so take enough rest after surgery
- You should avoid playing sports for a few days to protect the affected area, as too much jerk could dislodge the blood clot
- Drink lots of water to avoid dry mouth
- Avoid drinking alcoholic, carbonated, or hot drinks for 2-3 days
- Avoid eating anything that is hard for your wound
- Eat as per instruction, as acidic or spicy food could irritate your gums
- Practice standard oral care with recommended mouthwash
- Avoid touching areas around the affected area while brushing as this could dislodge the blood clot
- Don’t forget to visit your dentist, even if there is no complication.
What increases risk of dry socket?
The incidence rate of dry sockets is very low in the range of 2-3%. If you follow preventive measures, the chances of the dry sockets could be reduced to zero. The risk factor is relatively high among nicotine addicts, as nicotine reduces the blood supply thus prevents the formation of the blood clot. So, if you want to cut the risk of dry socket occurrence, you have to control nicotine consumption.
The risk is relatively high with the extraction of wisdom teeth, the third molar, as the extraction procedure requires the removal of some gum tissues and jawbone. The trauma can increase if the dry socket develops due to blood clot dislodgement.
The preexisting periodontal disease increases the chance of dry socket formation, as some bacteria are known for dissolving blood clots.
Studies suggest that women are more prone to dry sockets as compared to men. And one of the main reasons is the hormonal imbalance due to the menstrual cycle and the use of contraceptives. If you are in the 30+ year age group, the chance of developing a dry socket is high as dense jawbones make extraction traumatic, and less blood supply cuts the chance of blood clot formation.
Conclusion
Tooth extraction-induced trauma is unavoidable, but dry sockets could be prevented. All you need to do is follow standard oral care practices and avoid doing things which could affect blood clot. Dry socket condition develops within 2-3 days of extraction, so you should be cautious during the period to let your wound heal quickly. If you notice symptoms of dry socket development, you should consult your dentist, without delay. Ultimately it is all about keeping your dental system healthy, so why invite a painful dry socket, if you could prevent it from happening.
Sources:
- Cardoso, Camila Lopes, et al (2010). “Clinical concepts of dry socket.”
https://www.sciencedirect.com/science/article/pii/S0278239109018278 - Bowe, Denise C., Seamus Rogers, and Leo FA Stassen (2011). “The management of dry socket/alveolar osteitis.”
https://web.a.ebscohost.com/abstract? - Swanson, A. E. (1990) “Prevention of dry socket: an overview.”
https://www.sciencedirect.com/science/article/pii/003042209090104Z - Dodson, Tom (2013). “Prevention and treatment of dry socket.”
https://www.nature.com/articles/6400913 - Mamoun, John (2018). “Dry socket etiology, diagnosis, and clinical treatment techniques.”
https://synapse.koreamed.org/upload/SynapseData/PDFData/3070jkaoms/jkaoms-44-52.pdf